Mini-Brains Reveal New Insights Into Mitochondrial Brain Disorders
Summary: Researchers have created mini-brains to study how mitochondrial failure impacts brain cells, opening new possibilities for treating severe conditions like epilepsy. These brain organoids mimic real disease processes, allowing scientists to observe mitochondrial dysfunction and test potential treatments.
Beyond epilepsy, the research could improve understanding of conditions like Alzheimer’s and Parkinson’s diseases, which are also linked to mitochondrial issues. Mini-brains offer a powerful tool for studying disease progression, testing personalized therapies, and identifying novel drug targets.
Key Facts
- Mini-Brain Innovation: Mini-brains mimic mitochondrial dysfunction in brain diseases.
- Therapeutic Testing: They allow real-time study of disease progression and personalized treatments.
- Broader Impact: Findings could aid research on epilepsy, Alzheimer’s, and Parkinson’s diseases.
Source: University of Bergen
Researchers at the University of Bergen have used advanced stem cell technology to develop mini-brains, also called brain organoids, that can mimic disease processes caused by mitochondrial failure.
This could open new avenues for treating serious brain diseases such as epilepsy.
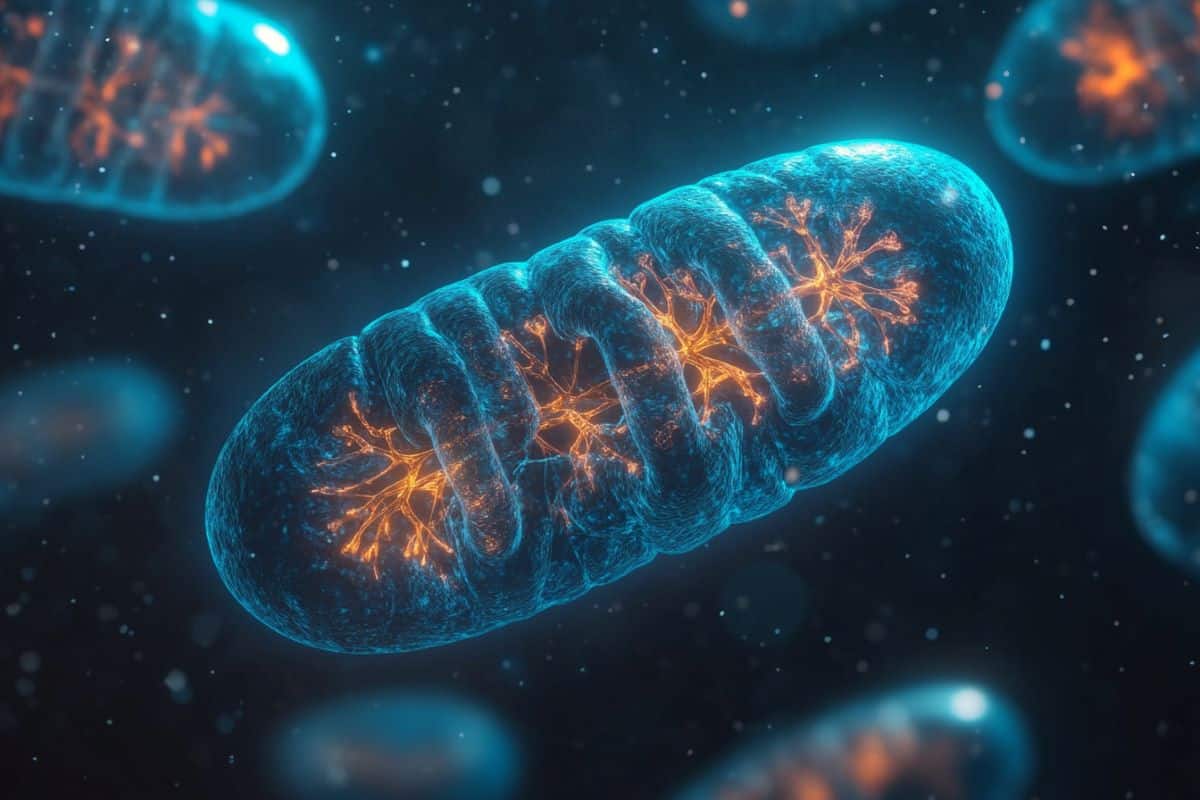
Mitochondria, known as the powerhouses of cells, are crucial for supplying the brain with energy. When mitochondrial function fails, this can lead to serious disorders in the brain, which require a lot of energy to function.
Using mini-brains, a research team led by Kristina Xiao Liang at the Department of Clinical Medicine, University of Bergen, has been able to study how genetic mutations in mitochondria affect brain cells and other cell types.
“The mini-brains give us a unique opportunity to understand disease mechanisms at the cellular level and test potential treatments. This is a significant step towards developing new therapies for diseases like severe epilepsy,” says Liang.
In addition, the research can contribute to a better understanding of other brain diseases such as Alzheimer’s and Parkinson’s disease.
The mini-brains offer a valuable model for exploring complex disease processes and testing treatment strategies in a realistic but controlled environment.
“These diseases often involve mitochondrial dysfunction that can be studied in the mini-brains. They allow researchers to study disease progression in real time, test personalized therapies, and identify new drug targets.
“While they are still under development, they have shown that we can increase our understanding and treatment of these conditions, potentially revolutionizing the field,” says Liang.
About this genetics and neurotech research news
Author: Paul Sommerfeldt
Source: University of Bergen
Contact: Paul Sommerfeldt – University of Bergen
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Hallmark Molecular and Pathological Features of POLG Disease are Recapitulated in Cerebral Organoids” by Kristina Xiao Liang et al. Advanced Science
Abstract
Hallmark Molecular and Pathological Features of POLG Disease are Recapitulated in Cerebral Organoids
In this research, a 3D brain organoid model is developed to study POLG-related encephalopathy, a mitochondrial disease stemming from POLG mutations.
Induced pluripotent stem cells (iPSCs) derived from patients with these mutations is utilized to generate cortical organoids, which exhibited typical features of the diseases with POLG mutations, such as altered morphology, neuronal loss, and mitochondiral DNA (mtDNA) depletion.
Significant dysregulation is also identified in pathways crucial for neuronal development and function, alongside upregulated NOTCH and JAK-STAT signaling pathways.
Metformin treatment ameliorated many of these abnormalities, except for the persistent affliction of inhibitory dopamine-glutamate (DA GLU) neurons.
This novel model effectively mirrors both the molecular and pathological attributes of diseases with POLG mutations, providing a valuable tool for mechanistic understanding and therapeutic screening for POLG-related disorders and other conditions characterized by compromised neuronal mtDNA maintenance and complex I deficiency.
Source link